April 6, 2018
Many practices in the US continue to use paper based methods for billing their patients and filing for claims even though their other management areas are electronic or cloud based. The case might be because of complicated medical billing process and too many components to handle. This article offers a lean solution for practice management systems to build tech enabled billing system for the benefit of their partnering practices.
Billing system:
a) Raising invoices for patients to make payments directly
b) Filing claims for insurance providers.
Core features:
Invoicing, Electronic filing, Clearinghouse integration, and Payment gateway
Overview of a lean billing system:
This connects the different entities such as patient, practice, clearinghouse involved in the billing process. At this stage, it is alright to not connect the insurance providers directly into your PMS as clearinghouse integration will be good enough.
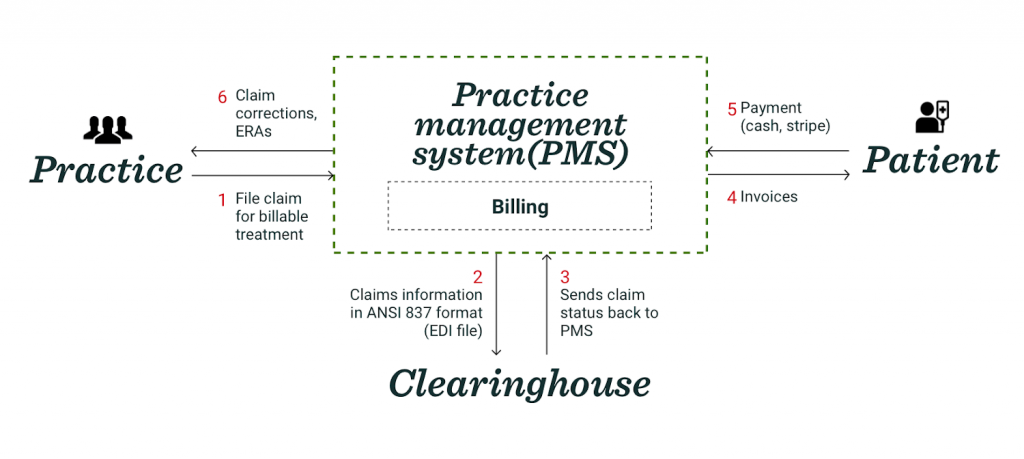
How it works
- Practices select the codes for billable treatments, and assemble the bill to be sent for insurance claim.
- Practice management systems will then send this claim file to a clearinghouse(more on choice of clearinghouse below) electronically via ANSI 837 format in an EDI file(more on EDI file below).
This shall also require enrollment in Medicare Electronic Data Interchange. - Status of the claim will be tracked. Rejected, denied and partially paid claims will be sent back to the system.
- Invoices to be generated from the application for the amount patients prefer to pay out of their pockets. This can also happen in the beginning of payment procedure as per policyholder.
- Accept payment through cash, stripe, or any other payment gateway integration. For cash, the system should allow the practices to track which bills are paid through cash.
- Based on the status and report(denied, rejected) received from the clearinghouse, practices will be able to edit/correct the claims and send it back.
A comprehensive billing system
Once the core elements are in place for a lean system, more comprehensive system can be built in later stages. Based on the medical billing process more features will make the billing procedure more robust.
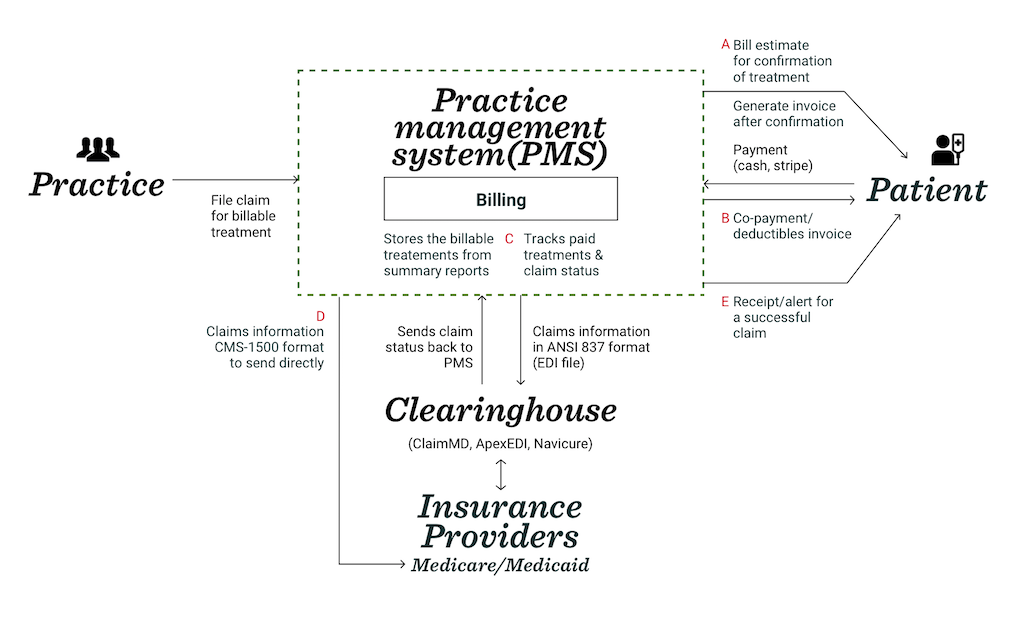
How it works
-
An initial bill estimate to be presented to the patient based on the diagnoses. Patient can choose which all treatments to go for. And invoice can be generated after the patient confirms, in case they are paying out of pocket.
Benefit: An early confirmation from the patients helps in getting payments more successfully. -
Invoices for the deductibles and co-payments to be raised for the patients, based on their insurance plans and coverage.
-
The billing section in practice management systems will import the billings codes and other treatment information to initiate claims filing. It will track the paid treatments and practices can view the claims status here.
-
Parallel to ANSI 837 format, claim filing to be done directly to Medicaid or Medicare using CSM-1500 format. Practices can upload a scan of the hard copy for this or send information electronically.
-
Once the payment is collected a confirmation should be sent to patients about the successful claims procedure.
Requirements for filing electronically
EDI file format for filing claims electronically
Converting the table data to EDI
Guide for 837 filing
Scanning hard copy for CMS-1500
Hard copy format of CSM-1500
Filing to clearinghouses
From the many options, Apex EDI stood out because of its cost, features, and the integration with the PMS so that the practices will not have to leave their PMS to process claims.
Navicure, Apex EDI and Claim MD are one of the best clearinghouses in market. They all provide ERAs and EOBs, allow corrections and resubmission of claims in real time, claims history and electronic filing.
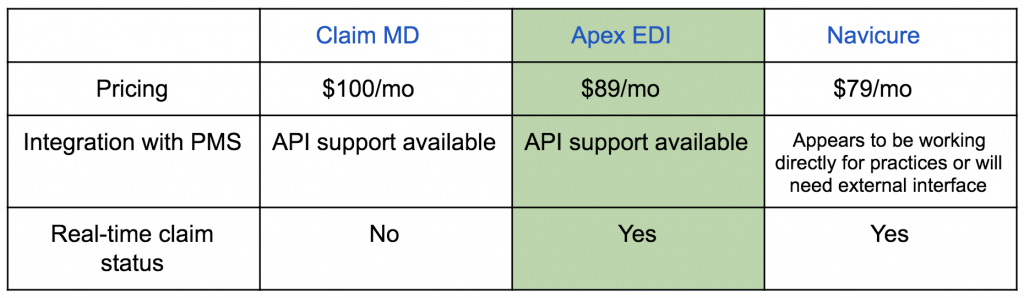
Though clearinghouses ensure insurance requirements and HIPAA compliance which reduce the potential for error dramatically, PMS can file the claims directly to insurance providers (I’ll be writing more on this).
Conclusion
A PMS can allow their practices with greater technological capability in carrying out medical procedures to save costs and effort on external billing methods. With a lean system, PMS can build the billing system faster and much closer to the needs of the practices.